Welcome to The Mindful Motion Physical Therapist Specialist
2023-11-06
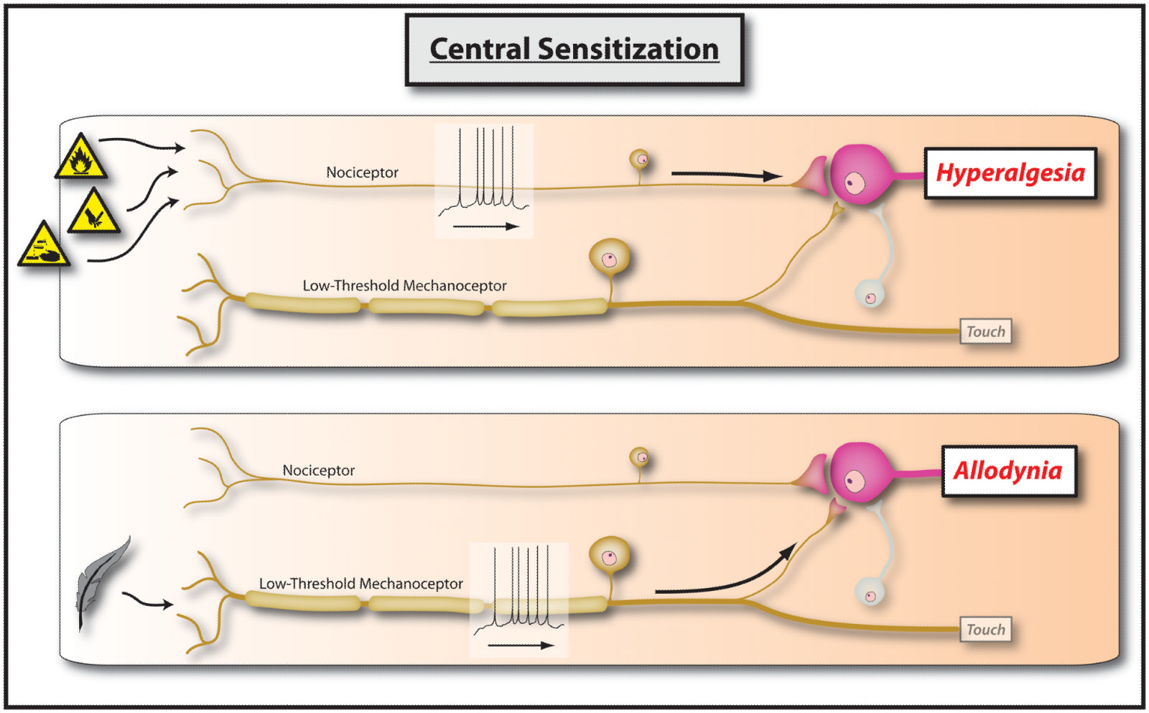
Central sensitization means hypersensitivity of the central nervous system (brain and spinal cord). Central sensitization is one of the reasons,but not the only reason, for the persistence of pain. Due to central sensitization there is a heightened response from the nervous system to any stimuli. Think about our nervous system as an alarm system. We need a sensitive alarm system to let us know that there is some threat or danger. Similarly, our nervous system warns about any danger or threat in our body. However, for some reason our body’s alarm system becomes faulty and oversensitive/hypersensitive resulting in pain perception despite absence of danger or threat or injury. This can lead to heightened state of awareness and alertness. Hypervigilance becomes the norm, and our body’s alarm system starts responding to non-threatening and non-harmful stimuli.
Central Sensitization has two main characteristics
1 Hyperalgesia
Hyperalgesia occurs when the stimuli, typically painful, generates more painful states. It is a heightened response to normal painful stimuli9. For example, a simple knee bumping to furniture generates mild pain but people with chronic pain experience sharp pain due to increased sensitivity of the nervous system. Due to hyper reactivity of the nervous system, pain gets amplified in chronic pain patients. Additionally, due to hypersensitivity, many chronic patients start experiencing pain beyond the initial injury site and this phenomenon is called secondary hyperalgesia.
2 Allodynia
Allodynia occurs when a normal sensation of touch generates a painful response. In patients experiencing chronic pain, a normal touch sensation is perceived as pain due to heightened reactivity of the nervous system9. Therefore, a normal massage or touch generates excruciating pain. Sometimes a comforter touching your skin can trigger a heightened response and you experience sharp pain. You wonder again, what did I do? You have not done anything, but due to hypersensitivity of the nervous system, there is an allodynic response.
The person in this state of allodynia and hyperalgesia starts to wonder if something is wrong with him, or feel that they are going crazy. Intellectually, people with chronic pain know that a slight touch or bump should not generate too much pain, but it does and this makes them think that something is damaged or wrong at the painful site. However, they are not going crazy or anything is damaged, it is their central nervous system which is extra sensitive to normal non threatening sensory stimuli.
Researchers have also found that other sensory stimuli like sound, odor and light can amplify their painful state2. Anecdotally, one of my patients reported that the tick sound of clock triggers her headache. Or sometimes a strong perfume might make their pain worse. Central sensitization is also associated with altered emotional response and has affected cognitive ability. More and more it has been found that central sensitization is found in most chronic pain conditions like fibromyalgia, chronic fatigue syndrome, whiplash injury, chronic neck and low back pain4,5,6,7.
What causes Central Sensitization?
Before we jump to central sensitization, first let us understand peripheral sensitization which can lead to central sensitization. I know, reading the word sensitization is making you sensitive, but hold on.
Any tissue injury results in an inflammatory process (this is the first step for the healing process) surrounding the injured site. Inflammation is nothing but the secretion of fluid and within this fluid there are certain chemicals released. Let's call this a chemical soup. The chemicals in this soup activate the special receptors/sensors called nociceptors, and simultaneously reduce the threshold of these receptors/sensors (which means these receptors get activated with a very low level of stimuli, think of a smoke alarm buzzing on burning a candle in the building. Before it required a huge fire to turn the smoke alarm, but now due to faulty wire connection or abnormality, it buzzes with mild smoke in the air).
[Side Note: Nociception is a neural process of coding and processing noxious (actual or potential tissue damaging event) stimuli. There are various nociceptors (special receptors or sensors to detect noxious stimuli) such as thermal receptors/sensors: which detects the changes in temperature, Mechanoreceptor/sensors: which detects the changes in the pressure and so on.]
Once these nociceptors are activated, the signal of nociception passes through specialized nerve fibers (originally thought to be pain fibers) and reaches the dorsal horn (region in the spinal cord) of the spinal cord. The signal from the spinal cord is relayed to the different areas of the brain.
Persistent inflammation at the injured site can constantly activate the nociceptors resulting in the hypersensitivity of these receptors/sensors leading to activation of these sensors randomly without any noxious stimuli8. This is called peripheral sensitization. Peripheral sensitization can lead to increased nociceptive input to the spinal cord. Research has suggested reversible changes occur in the cells of the dorsal horn of the spinal cord due to constant nociceptive input from the periphery.
Now as we know from the previous blog, the signal from the spinal cord reaches various parts of the brain and the brain ultimately decides that it is worth being in pain or not.
Once the nociceptive input reaches the spinal cord and then it is relayed to the higher centers in the brain. Based on analysis by brain region, descending inhibitory signals (dampening) or descending facilitating signals (amplifying) are sent to the spinal cord. If there is less inhibiting and more facilitating signals are sent to the spinal cord, it can result in more excitability and heightened response aka more pain.
Central nervous system has a property of plasticity called neuroplasticity, which means the nervous system constantly changes or modulates based on different sensory and motor experiences. The simplest form of plasticity in the nervous system is that repeated noxious stimuli can lead to habituation (reduced response) or sensitization (increased response)8. In chronic pain patients, repeated noxious stimuli results in sensitization or heightened response resulting in hyperexcitability of the nervous system. This is termed as Central Sensitization.
Thus central sensitization is the result of changes in excitability and heightened response of neurons (cells in brain) in the central nervous system, pain is no longer coupled, as is the case with acute nociception is, with the presence, intensity and duration of initial peripheral noxious stimuli8. For this reason, traditional treatment to manage chronic pain is ineffective.
So what should be the treatment of chronic pain
Treatment of Chronic Pain
It is a multidisciplinary approach to manage chronic pain,starting with in-depth explanation to the patient about current pain science. Education is a very crucial step in chronic pain management because most of the patients still believe that their pain is related to some damage in the body, even though the injury occurred many months or years ago beyond the healing time of injured tissue11. Combination of cognitive behavioral therapy (CBT) and traditional physical therapy has proven to be effective in managing chronic pain10